All infusion centers share the common goal of providing services to meet the needs of as many patients as possible. Before optimal patient scheduling can occur, however, an infusion center must first determine its maximum capacity.
Determining an infusion center’s maximum capacity entails two key steps. First is the calculation of a center’s theoretical maximum capacity. Then, as became especially critical in the last two years, there is the factoring in of real-world circumstances that affect how much of the theoretical maximum capacity can truly be captured.
Calculating theoretical maximum capacity of the infusion center
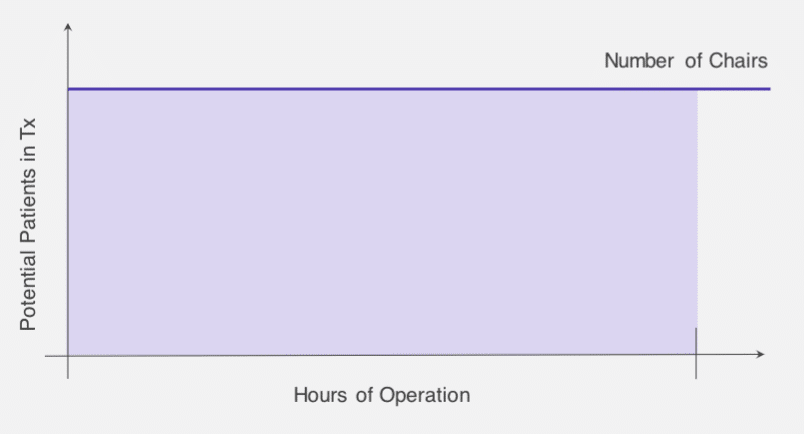
Calculating an infusion center’s theoretical maximum capacity is a straightforward equation: Total Available Chair Hours = Hours of Operations x Chair Count
Total Available Chair Hours is a good starting point in defining a theoretical upper bound to maximize infusion center capacity. A center simply cannot deliver more patient hours than what chair hour capacity can accommodate. This is a relatively fixed capacity unless the center is willing and able to make the capital investment of adding chairs and, if necessary, additional space, and/or make the operational investment of increasing hours of operation.
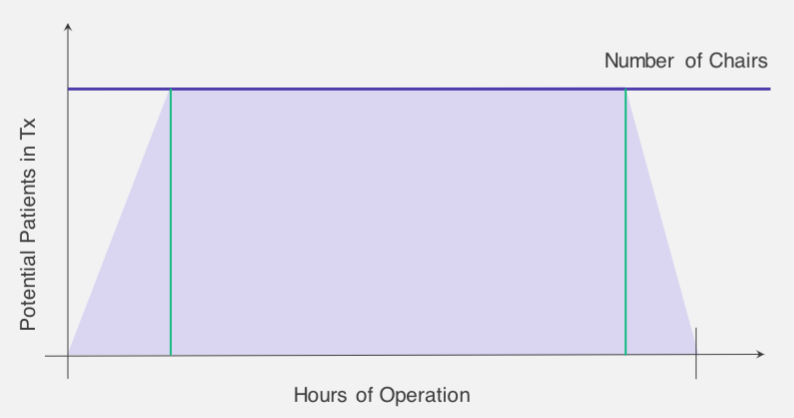
At its simplest, the two fundamental levers to push and pull on to impact Total Available Chair Hours are infusion chairs and operating hours. Nursing hours and pharmacy resources are additional key variables. Using basic geometry, the maximum capacity for an infusion center can be represented by the area of the rectangle below.
Importantly, it is never feasible for an infusion center to operate at 100 percent of its theoretical maximum capacity. Doing so would require starting as many patients as a facility has chairs the first thing in the morning, and then keeping every single chair occupied and in-service throughout the entire day, and obviously this is not a feasible way to maximize infusion center capacity. Not only does that model not take into consideration the inherent variability of infusion treatments, operationally it requires having the same number of nurses as there are chairs. Since one nurse can only start the treatment for one patient at a time, 15 chairs would require 15 nurses to run them all simultaneously at full capacity. Especially at a time of staff shortage, doing so is simply not possible.
Understanding what optimal infusion center capacity means
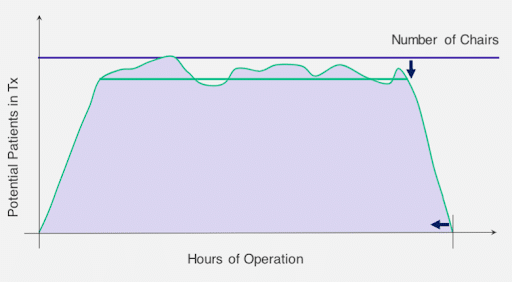
As it’s not feasible to operate at a theoretical maximum capacity, the key to operating at an optimal infusion capacity involves “shaving off” parts of the theoretical capacity that are not capturable, to discover the true capacity that can be utilized.
The first cut into capacity is the determination of ramp up speed, or how long it takes to reach full capacity at the start of the day. Factors of ramp up speed include:
- Nurse staffing (number of nurses available at each point throughout the morning, and the amount of time needed to start each patient)
- Lab availability and capacity
- Pharmacy availability and capacity
As it relates to ramp up speed for the infusion center, the capacities of both the lab and the pharmacy are constraints. For example, if an infusion center’s pharmacy has the capacity to mix the drugs for a maximum of eight regimens per hour, then an infusion center overall cannot ramp up any faster than that.
With the impact of resource constraints, the best method to determine ramp up speed is to follow the best case scenario, analyzing the data from recent days that were ramped up the mostly quickly and applying those results to optimal capacity calculations.
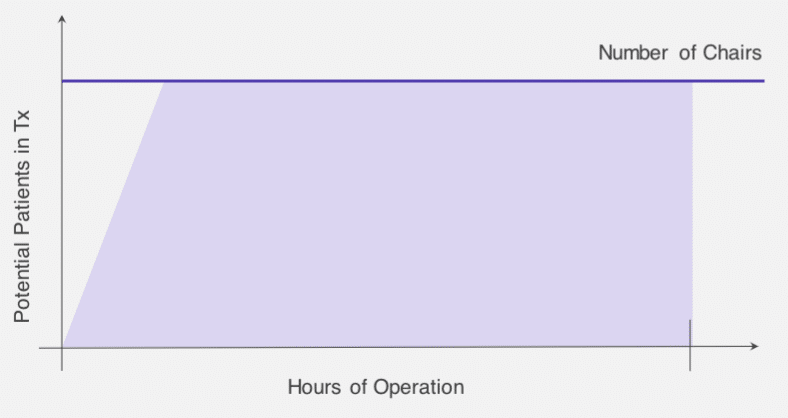
In addition to impacting ramp up speed, available nursing resources are essential to determining volume goals, with touch time, headcount-to-patient ratios, and expectations of patients seen per shift each playing a part. Touch time is the amount of time a nurse needs to get started with a patient, and it directly impacts the ramp up speed that is possible. Established nurse headcount-to-patient ratios imply the number of chairs that can be utilized during fully staffed portions of the day, which may be less than the physical chair count. For example, if guidelines suggest a nurse can adequately serve four patients at a time, a facility with 10 nurses could serve a maximum of 40 patients at one particular time during the day, regardless of whether 50 chairs are available. Lastly, the expectations for the number of patients seen per nursing shift is another limiting factor; if there’s an upper limit of 8 patients seen per nurse and there are 10 nursing shifts, the capacity is limited to 80 patients.
The second shaving cut into infusion scheduling capacity involves the consideration of ramping down at the end of a day. Ramp down speed is a function of the following:
- Number of nurses available at each point throughout the afternoon and the amount of time needed for patient disposition
- Last appointment start time
- Pharmacy availability and capacity
An infusion center will never have all of its chairs full until closing time, but how deeply the ramp down cuts into capacity can be influenced by adjusting the factors above. Managers can evaluate the impact of adjusting the final appointment start time or an extension of pharmacy availability to determine if a positive return on investment can be realized by stretching available capacity.
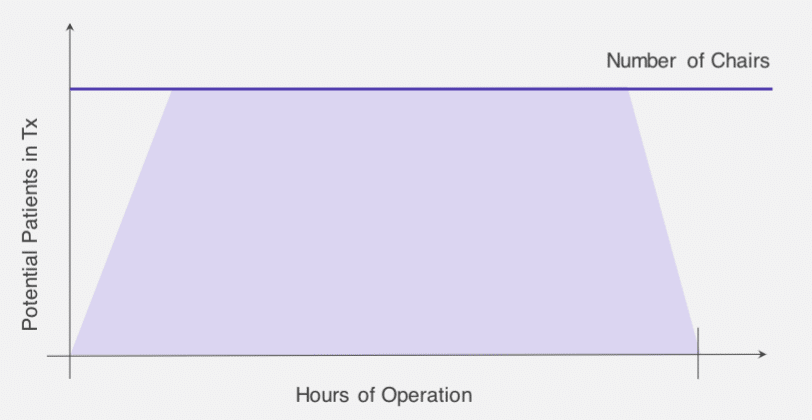
Calculating effective infusion center capacity
Once an infusion center has shaped its theoretical capacity into a more realistic effective capacity by adjusting for ramp up and ramp down time, based on historical data and assumptions that are safe, reasonable, and achievable, schedulers can begin to calculate the capacity available and place appointments to fit the space.
Thus far, we’ve thought of the capturable capacity of the infusion center as essentially the area of the trapezoid in the graph below, which we can easily calculate by summing the area of the ramp up time, the ramp down time, and the rest of the day in between.
But the capacity in terms of patient hours still isn’t the answer an infusion scheduler needs to actually maximize infusion center capacity. Determining the number of patients that can be scheduled into this shape can be estimated quickly by dividing patient hours by the average treatment length.
A more precise calculation involves a typical daily mix of appointment lengths – one hour appointments, two hours, three hours, etc. – and scaling that mix until it reaches the number of patient hours previously calculated.
A final consideration is the variability of the day, caused by add-on cases, no-show appointments, allergic reactions, patients who have unexpected reactions or need more fluids, or any of the myriad of situations that can affect patient hour capacity. One way to estimate variability is to examine historical data and contrast actual chair utilization with scheduled chair utilization. Typically, those analyses show a degree of overutilization with regards to planned or budgeted time. In those cases it’s wise to insert buffer time and schedule into fewer chairs than the total number available.
If an infusion center is changing its schedule substantially, historical data may not be predictive of future variability. In those cases, a more precise forecast requires running simulations over a proposed schedule. Simulations can be run through a solution like LeanTaaS’ iQueue for Infusion Centers.
A simulation should effectively identify patterns in historical data and then measure the impact of those repeatable patterns over a proposed schedule. The number of buffer chairs needed depends on the level of variability in infusion operations, and the three most important variations to consider are:
- Variation in patient arrival time
- Room-in variation, or the wait time due to operational delays
- Room-out variation, or the variation in treatment length
Steps to maximize infusion scheduling capacity
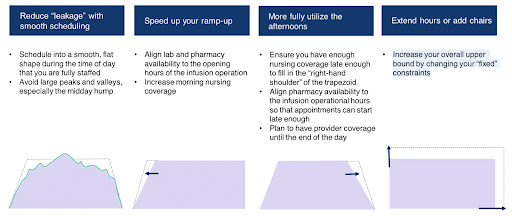
When looking to optimally schedule, it’s important to schedule to effective capacity, not theoretical capacity. But it is possible to expand an infusion center’s effective capacity to better accommodate the needs of patients and providers. The best practices for maximizing effective capacity include:
- Smooth out scheduling. When the infusion center is staffed as fully as possible, avoid large peaks and valleys in patient hours scheduled, especially during the common 10am to 2pm midday “peak”.
- Speed the daily ramp up time. Align lab and pharmacy availability to the opening hours of the infusion operation, and optimize morning nursing coverage.
- Shorten ramp down time to better utilize the afternoon. Ensure sufficient nursing coverage at the end of the day, align pharmacy availability to the infusion operational hours so that appointments can start late in the afternoon, and plan to have provider coverage until the end of the day.
- Extend hours or add chairs. Increase overall upper theoretical capacity limitations by changing previously fixed constraints.
To learn more about adjusting operational factors to maximize infusion center capacity, see iQueue for Infusion Centers or visit our infusion Resource page.